Guide to Preventing Alzheimer's
What are BAT Levels?
The Silent Threat You Can't Ignore
What are Alzheimer's Biomarkers?
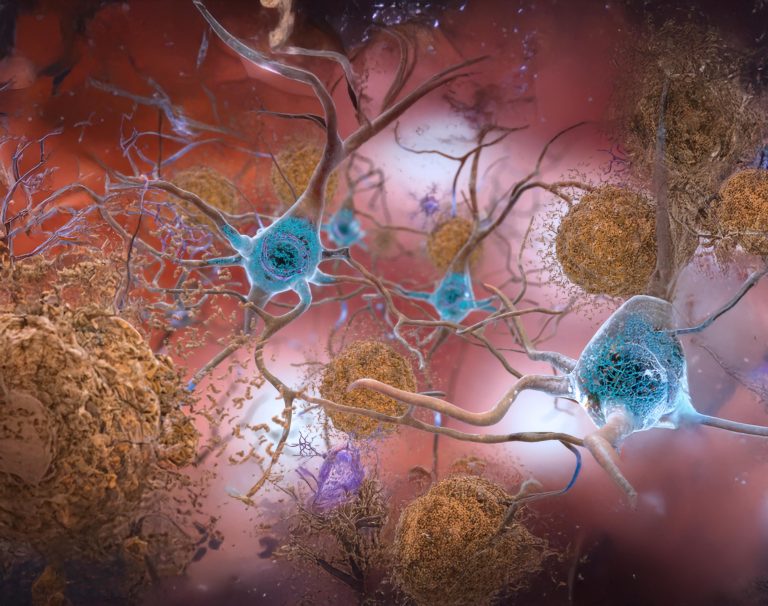
Scientific advancements have allowed us to detect the earliest signs of Alzheimer’s through biomarker testing—well before symptoms begin. The two hallmark biomarkers of Alzheimer’s Disease are:
- Beta-Amyloid 42/40 Ratio: Indicates early plaque formation in the brain, which can begin accumulating as early as 20 years before symptoms.
- Phosphorylated Tau (pTau 181, 217): A marker of neurofibrillary tangles, which directly correlates with cognitive decline and neuron loss.
These levels of these two markers, Beta-Amyloid and Tau (BAT) Levels, are the foundation of Alzheimer’s pathology.
Understanding BAT Levels as the Primary Risk Factor
BAT Levels do not cause immediate symptoms but are the #1 modifiable risk factor for Alzheimer’s progression. Their accumulation creates a silent risk—much like how high cholesterol signals heart disease risk.
Key Facts About BAT Levels:
- Beta-Amyloid (BA) builds up first, Tau follows. BA accumulation begins decades before cognitive symptoms appear, eventually leading to Tau formation, which triggers active neuron loss.
- Not everyone with elevated BA Levels will develop Alzheimer’s—but without intervention, the risk increases dramatically.
- High BAT Levels are treatable. Unlike genetic risks (such as APOE4), BAT Levels can be monitored, reduced, and controlled with targeted interventions.
We have compiled a graph below using all of this data to illustrate the progression of various biomarkers of Alzheimer’s disease over time, starting from the preclinical stage through to dementia.
Here below are the key observations:

• Red Line (Beta-Amyloid Accumulation): Starts in late 30s to early 40s, peaking by mid-50s.
• Green Line (Tau Accumulation): Begins in mid-40s, with significant levels by early 50s, indicating neuronal damage.
• Blue Line (Brain Structure Changes): Detectable in early 50s, reinforcing the need for early BAT Testing.
• Purple Line (Cognitive Changes) &Yellow Line (Clinical Symptoms): Begin mid-60s, progressing to diagnosis by 70-75.
Mechanisms that Lead to BAT Levels
Inflammation & Immune Dysregulation
(Neuroinflammation)
Chronic inflammation triggers immune responses that impair the brain’s ability to clear BA aggregates.
Elevated C-reactive protein (CRP), ESR, and cytokines correlate with increased risk of Alzheimer’s.
Autoimmune conditions (such as rheumatoid arthritis, lupus, and MS) lead to persistent inflammation, accelerating BA accumulation.
Lipid Transport Dysfunction
(Cardiovascular Risk)
The brain relies on lipoproteins (such as APOE) to clear beta-amyloid.
Dysregulated lipid metabolism (high LDL, low HDL, or elevated homocysteine) slows BA clearance, leading to accumulation.
Statins and lipid-modulating treatments may play a preventive role by improving BA clearance.
Glucose Dysregulation & Metabolic Dysfunction
(Diabetes & Insulin Resistance)
Diabetes and metabolic syndrome impair insulin signaling in the brain, contributing to amyloid plaque formation.
HbA1c levels and insulin resistance markers correlate with higher BA deposition in at-risk patients.
Patients with Type 2 Diabetes have a 2x increased risk of Alzheimer’s, emphasizing the need for early metabolic screening.
Chronic Stress & HPA Axis Dysfunction
Elevated cortisol levels (chronic stress) damage neurons and increase BA deposition.
Cortisol impairs autophagy, the natural process that clears misfolded proteins.
Long-term stress exposure accelerates cognitive decline and tau pathology.
Iron Overload & Oxidative Stress
Excess iron accumulation in the brain catalyzes oxidative damage, promoting BA aggregation.
High ferritin levels are associated with faster Alzheimer’s progression.
Iron dysregulation is a key modifiable mechanism that contributes to neurodegeneration.
All Roads Lead to BAT Levels
Each of these processes leads to the same endpoint—increased beta-amyloid burden. This is why BATWatch testing includes a Mechanism Panel (MP) to assess these contributors before BA accumulation becomes irreversible.
How are BAT Levels Tested?
While spinal fluid tests and brain scans are options, they’re expensive and invasive. The BATWatch Protocol takes a different approach, utilizing a simple, cost-effective blood test with a structured multi-test process to ensure accuracy and reliability.
